Helping parents of neurodivergent children reduce mealtime stress and expand food variety.
Helping neurodivergent children with autism, ADHD, and restrictive eating feel confident around food by supporting parents with practical, dietitian-led feeding guidance.
If mealtimes are filled with anxiety, sensory overwhelm, or nutrition worries, you are not alone. I help families to feel confident feeding their child.
If you are looking for simple steps that make a real difference, this is where to begin.
I went from feeling helpless watching meals go untouched to creating mealtimes where kids explore food willingly.
kristy jordan
dietitian & feeding therapist
Hi, I'm Kristy!
I know how exhausting and disheartening mealtimes can feel, especially when your child is autistic and food feels like a daily battle. I’ve seen the stress, the worry, and the frustration when every strategy seems to fall short.
Through years of working alongside families as a feeding therapist, I’ve learned how to create a mealtime environment that encourages eating. My approach helps children feel safe exploring food at their own pace, while giving parents the tools and confidence to support them without pressure.
I’ve walked with many families of autistic children as they’ve rebuilt trust at the table, celebrated progress, and rediscovered joy in mealtimes - and I’d love to help you do the same.

Support your child’s health and development by making achievable progress with food today
Are you worried about your child's nutrition?
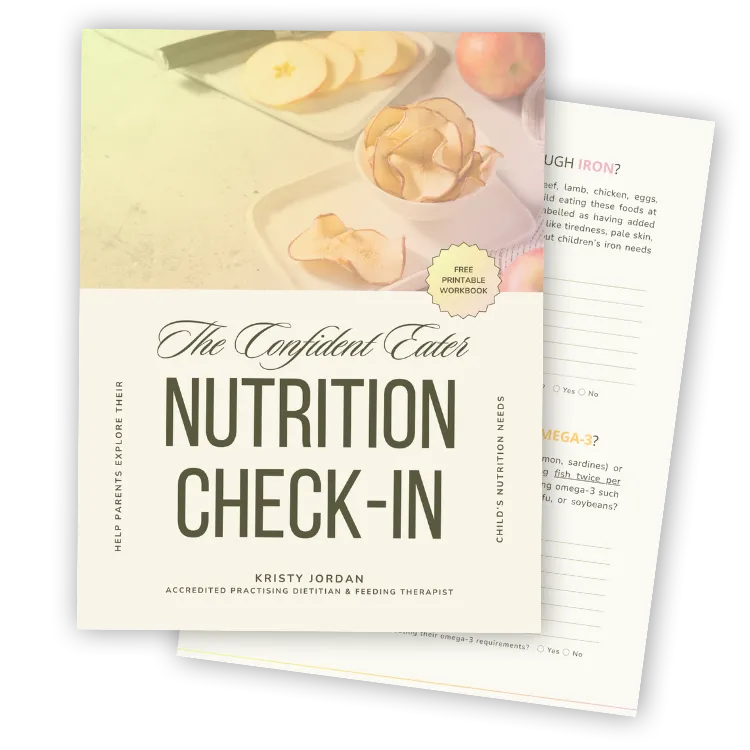
A free, printable workbook for parents
How many times have you wanted to feel confident about your child’s nutrition, but felt stuck between worrying too much and avoiding thinking about it altogether?
If your child eats a limited range of foods, it is natural to wonder whether they are getting what they need.
This Nutrition Check-In is designed to help you understand where your child’s intake may already be okay, and where extra support might be helpful.
Ready to build the family meals of your dreams?

Join The Community
Get guidance from experts and join a supportive community of parents who understand. Together, we’ll help you create a mealtime environment where your child's needs are being met, and you can relax knowing you are doing everything you can to support them in their journey.
Follow Me On Instagram
Get daily tips, inspiration, and behind-the-scenes insights to help you stay motivated and improve your relationship with your child at mealtimes.
Subscribe To The Newsletter
Subscribe to the Grate Adventure newsletter for actionable strategies, expert advice, and inspiring stories to help you to learn what changes you can make to help your child, starting today.
Are you ready for more?
Ready to build the life of your dreams?

Let's chat
Ready to work with a coach to uplevel your life and business?
Listen to the
Podcast
view my
services
read the
BLOG
Let's chat
Ready to work with a coach to uplevel your life and business?
Let's learn
Learn at your own pace and make quantum leaps.
Student Love Notes
We've helped so many incredible students to find success as Virtual Assistants...

The VA Business Blueprint helped me to go from feeling completely stuck to starting my business and getting my first client!
Ellen, business name

I enrolled in the VA Services Academy feeling completely lost - within 2 weeks I knew exactly what to offer & what to charge.
Ellen, business name

Beginner to Booked Out was a game-changer for me. Anna and her team are incredible and I'm booked out for the next 3 months!
Ellen, business name
New on the blog...

Dinner Without Drama: A 5-Day Reset for Calmer, Happier Mealtimes

What Happens When Your Child Doesn’t Eat? How Food Affects Your Mood

Constipation in Neurodivergent Children: A Practical Guide for Parents
New on the blog...

Constipation in Neurodivergent Children: A Practical Guide for Parents
Constipation is common in children - especially those who are neurodivergent - and can affect everything from appetite to behaviour. In this article, I explore what constipation looks like, why it happens, and how to support healthy, comfortable bowel habits at home. You will learn about dietary strategies, hydration, toilet posture, and when to seek medical advice.
Signs and symptoms of constipation
Constipation refers to hard, dry or difficult-to-pass stools, or withholding behaviours, rather than a specific number of bowel motions.
Typical signs and symptoms you may observe include:
Stomach cramps or intermittent abdominal pain – children may complain of tummy ache or pull their legs up.
Reduced appetite – if the child feels bloated or backed-up, they may eat less.
Irritable or changed behaviour – pain or discomfort around bowel movements may cause avoidance or mood change.
“Holding-on” behaviours – such as squatting, crossing legs, refusing to sit on the toilet, hiding or delaying going to the loo.
Hard lumps of stool or feeling a firm mass in the lower abdomen when gently pressed.
Soiling or “accidental” leakage (sometimes soft or runny stool leaking around a mass of impacted stool) – medically called encopresis.
Because neurodivergent children may have sensory differences, communication differences or toileting anxiety, the above signs may present in different ways (e.g., non-verbal indication of pain, or refusal to use certain toilets). Noticing these behaviours early supports timely intervention.
Bristol stool chart
The Bristol Stool Chart (also called the Bristol Stool Form Scale) is a useful visual tool to help caregivers and clinicians assess stool consistency rather than focusing on frequency alone.

What is ideal?
Types 1–2: separate hard lumps (like nuts) or sausage-shaped but lumpy suggest constipation.
Types 3–4: like a sausage or snake, smooth and soft is considered “ideal”.
Types 5–7: softer blobs (easy to pass) from mushy through to watery may indicate faster transit or diarrhoea.
3. What causes constipation
In children, most constipation is “functional” – meaning there is no underlying structural or disease cause, but rather bowel habits, diet, toileting behaviours and physical factors.
Common causes/risk-factors include:
Slow gut movement or a natural tendency toward harder stools.
Withholding behaviours: if a child delays pooing because of pain (anal fissure) or fear (toilet environment) it leads to bigger, harder stools, and a cycle of avoidance.
Changes in toilet environment or routine: starting school, using unfamiliar/uncomfortable toilets, busy playtime, sensory issues around toileting.
Diet: low fibre intake, low fluid intake.
Low physical activity.
Because children who are neurodivergent may have sensory or behavioural differences around toileting, holding-on, or differences in awareness of bodily signals, extra attention to toileting opportunities, comfortable toilets and consistent routines is often helpful.
Food remedies for constipation
Here are some dietary and fluid strategies that may support bowel regularity.
A reminder: this is general educational information (not personalised therapy).
1. High-fibre foods
Dietary fibre is the non-digested portion of plant foods that reaches the colon and helps by bulking up stool, softening it and stimulating gut motility via fermentation.
Soluble fibre dissolves in water to form a gel-like substance in the gut. This gel traps water inside the stool, making it softer and easier to pass. It also slows digestion slightly, which helps regulate bowel movement consistency.
Good sources of soluble fibre include:
Oats and oat bran
Psyllium husk (Metamucil, Benefiber)
Legumes (lentils, chickpeas, beans)
Fruit such as apples, pears, kiwi, and citrus
Root vegetables such as carrot and sweet potato
By contrast, insoluble fibre (in wheat bran, whole grains, nuts, and vegetable skins) adds bulk and helps move stool through the bowel.
For constipation, a mix of both types is ideal - soluble fibre to soften, and insoluble fibre to stimulate movement.
2. Kiwifruit
Research in adults suggests that eating whole kiwifruit (green or gold) can increase bowel movement frequency, soften stools and reduce straining. While most studies are in adults, the mechanisms are relevant: kiwifruit provides fibre, helps water-holding capacity of stool and may stimulate gut motility. For children, offering 1–2 kiwifruit per day (if they tolerate the taste/texture) is a gentle, whole-food option.
3. Prunes
Prunes (dried plums) are a well-studied remedy for constipation because they contain sorbitol (a natural sugar alcohol) which draws water into the colon and helps stool pass. In a study comparing prunes to psyllium (fibre supplement), prunes increased bowel motion frequency and improved stool form. For children, offering a small serve of prunes (or prune juice diluted) can be helpful.
4. Water (fluids)
Fluid intake is vital because fibre needs water to work. When there is insufficient fluid, stool becomes harder and takes longer to pass. For children, encourage water through the day (e.g., water bottle accessible, fun straws or favourite cup), include hydrating foods (watery fruits/veggies). For neurodivergent children, visual prompts or routine drink times may help.
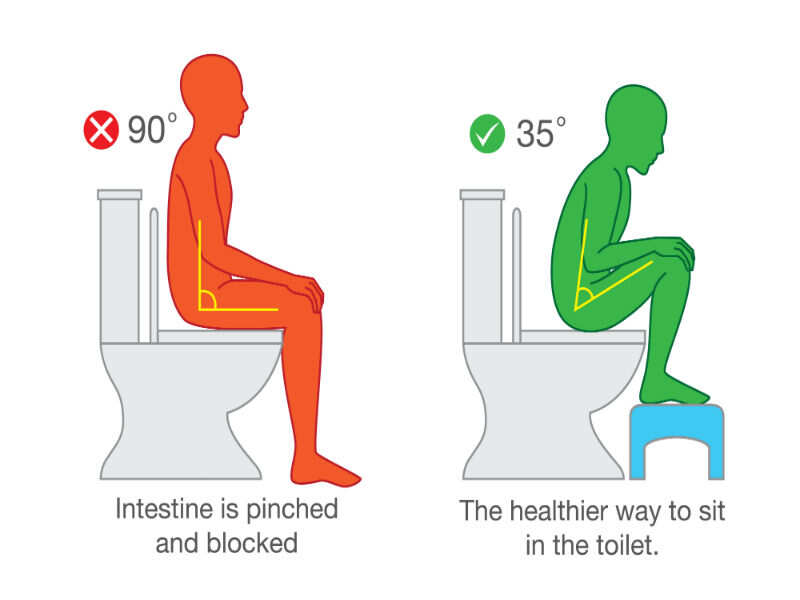
5. How to sit on the toilet
Effective toilet posture and routine matter because positioning strongly influences how easily the bowel can empty. Research and clinical guidelines highlight posture to support pelvic-floor relaxation and efficient rectal emptying.
Key tips for children:
Use a foot-stool so that the child’s knees are at the same height, or higher than their hips. This creates a “squatting”-like position which straightens the rectum and helps emptying.
Lean slightly forward, elbows on knees (or hands on thighs) – this helps open the rectum.
Keep the back straight (not slumped) – maintain a supportive posture.
Encourage abdominal breathing: breathe deeply, expand tummy, relax the anal sphincter rather than tighten. Avoid the child straining.
Set a toileting routine: after breakfast (due to gastro-colic reflex), and possibly after lunch/dinner. Encourage sitting for 2–3 minutes even if no immediate urge. Use a timer if helpful. Recognise that anxiety, avoidance or sensory discomfort can interfere with the mechanics of emptying.

6. When to see a doctor
Although many cases of constipation resolve with routine changes, there are times when medical review is warranted.You should consider consulting a doctor when:
The constipation has been going on for several weeks or months, despite diet/fluid/toileting changes.
There is blood in the stool (not just a little from straining or a visible fissure), or significant pain on toileting.
Soiling or leakage (encopresis) is occurring regularly (especially if rectal mass is felt).
There are “red-flags” such as unexplained weight loss, vomiting, or the child is very unwell.
The child has severe pain, or the bowel appears full and hard (suggesting impaction).
When you do visit a doctor, bring along a record of toileting habits (frequency, stool form via Bristol chart, withholding behaviours), diet/fluid patterns, and any toileting environment issues. For neurodivergent children, mention any sensory/toileting-anxiety factors.
References
Bae, S. H. (2014). Diets for Constipation. PMC. PMC
Eltorki, M., et al. (2022). Kiwifruit and Kiwifruit Extracts for Treatment of Constipation. PMC. PMC
“Childhood constipation” (2017). Australian Family Physician. RACGP
“Clinical Practice Guidelines: Constipation” (RCH). Royal Children's Hospital
ERIC. (2022). Constipation in children: symptoms, causes and relief. ERIC
“Constipation – Factsheet” (SCHN NSW). schn.health.nsw.gov.au
“Constipation and children” (Better Health Victoria). Better Health Channel
Bristol Stool Chart. Continence Foundation of Australia. Continence Health Australia
“Emergency management in children: Constipation” (PCH WA). Perth Children's Hospital
Have Questions or Need Support?
If you are worried about your child’s bowel habits, or if constipation seems to be affecting their comfort, appetite, or mealtime experiences, please reach out. Every child’s situation is different - especially for those who are neurodivergent - and it can make a big difference to have personalised guidance.
You can get in touch through Grate Adventures to ask a question, book a consultation, or join our Feeding Therapy Community for extra support and resources.